Most coughs aren’t usually serious and go away within a few days. They are the body’s natural way of responding to something that irritates the airways. It helps to clear mucus and foreign particles from the airways, thereby preventing infection and inflammation of the lungs. This process is initiated by stimulating the larynx (voice box) and the nerves of the respiratory tract.
But what if you have a cough that won’t seem to go away? While many individuals may not usually worry about a cough arising from a cold or the flu, it is advisable to seek medical attention if your cough lingers on for more than three weeks. It is particularly important to see your doctor when the coughing is prolonged or severe, accompanied by thick, greenish yellow phlegm or blood, or if you have breathing difficulties, fever and/or chest pain. Cough can be a symptom of a more serious underlying condition and as such, a lingering cough should never be ignored. Early detection and intervention can certainly help better manage the symptoms with improved quality of life and a better medical outcome.
Depending on the severity, your general practitioner (GP) may refer you to a respiratory specialist.
Coughs can be categorised according to the duration — acute, sub-acute, and chronic. An acute cough is a cough that lasts less than three weeks; a subacute cough, on the other hand, lasts between three to eight weeks. A cough is referred to as chronic if it lasts more than eight weeks. This classification is important — the duration of the cough at the time of presentation can help determine the likely causes.

What are the main causes of a chronic cough?
A persistent cough can occur due to a range of reasons. Some of the most common causes of chronic cough include:
- Asthma: This is a common lung condition that causes the airway to narrow, which makes it difficult for the patient to breathe.
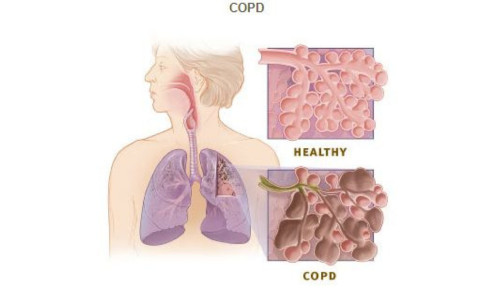
- Chronic Obstructive Pulmonary Disease: COPD refers to a group of lung diseases that cause breathing difficulties.
- COVID-19: This contagious disease is caused by the SARS-CoV-2 virus.
- Gastroesophageal disease (GERD): This condition occurs when stomach acid and contents are regurgitated into the throat and mouth; this is also commonly known as chronic acid reflux.
- Infections: Cough may present as a symptom of some respiratory infections such as pneumonia or whooping cough.
- Lung cancer: A worsening or prolonged cough may present in patients with lung cancer. It may start as a dry cough and progress to shortness of breath and coughing blood.
- Medications: Certain drugs, such as angiotensin-converting enzyme inhibitors (ACEIs) have been known to cause chronic coughs.
- Postnasal drip: This condition may lead to the constant sensation of wanting to clear your throat, with time this may lead to a chronic cough.
- Smoking: Smoke from cigarettes contains toxins that damage the airways and cause chronic coughing.
When do you need to see a doctor?
Although many cases of chronic cough may not be serious, some may warrant immediate medical attention. The warning signs and symptoms include:
- High fever
- Shortness of breath
- Chest pain
- Wheezing
- Copious sputum production
- Fatigue
- Night sweats
- Loss of appetite
- Coughing up blood
- Unintended weight loss
How is chronic cough treated?
First, your doctor will take your medical history and perform a physical examination. Investigations, may include:
- Laboratory tests (a sample of blood or phlegm will be tested for the presence of bacteria)
- Lung function tests (such as spirometry or cardiopulmonary exercise test)
- Imaging tests (may include chest X-rays, Ultrasound testing, CT, and MRI scans)
A high-quality digital chest X-ray (done in posterior anterior and left lateral position) can usually suggest conditions like:
- Lung cancer
- Metastatic cancer (cancer from elsewhere spreading to the lung)
- Bronchiectasis
- Active pulmonary tuberculosis
- Idiopathic pulmonary fibrosis
- Chronic obstructive pulmonary disease (COPD)
Sometimes, a CT scan of the thorax is done to clarify the chest X-ray abnormality.
In some cases, the doctor may recommend scope tests such as Bronchoscopy and Rhinoscopy. If needed, the doctor may also perform a biopsy to look for any abnormalities in the airway.
If the Chest X-ray is normal, the usual causes of chronic cough are:
- Cigarette smoking
- Post nasal drip due to allergic rhinitis
- Asthma
- Gastroesophageal reflux
- Drugs e.g., ACE inhibitors prescribed for hypertension
Treatment will depend on the findings of the investigations and may, for most cases, include:
- Decongestants, antihistamines, and corticosteroids — the standard treatment for a runny nose and allergy symptoms.
- Cough suppressants — to get relief from the cough
- Nasal sprays — for allergies and sneezing
- Antibiotics — for infections such as sinusitis or bacterial pneumonia
- Acid blockers — this medication may be given to patients with acid reflux
To quicken the recovery process, your doctor may also suggest the following advice:
- Drink plenty of water (at least eight glasses per day)
- Avoid certain foods and prop up your head during sleep (to reduce acid reflux)
- Avoid environments with dust and toxic fumes
- Avoid tobacco smoke
What are the complications and risk factors of chronic cough?
Smoking is one of the main risk factors for chronic cough. Other common risk factors include allergies, air pollution, and infections. Frequent exposure to these factors can result in severe consequences such as lung damage.
Patients with persistent coughs have a higher risk of developing several complications like headaches, sleep disruption, dizziness, fainting, and urinary incontinence (loss of bladder control). In addition, coughing may occasionally lead to fractured ribs in some cases.
How to avoid chronic cough?
First of all, it isn’t necessarily possible to avoid a cough since it is a symptom of several conditions, and coughs are the body’s reflex action. However, there are a few things that you can do to reduce the risk:
- Smoking cessation (smoking is the most common cause of chronic cough)
- Avoid secondhand smoke
- Avoid toxic fumes or pollutants
- Eat plenty of fruit and fibre-rich food and stay hydrated
- Avoid contact with anyone with a respiratory infection such as pneumonia or bronchitis
How can chronic cough impact your life?
It is well known that a persistent cough can negatively affect one’s health and well-being. With early intervention and following a consistent treatment plan, patients can avoid progression of illness, find relief from their symptoms, and enjoy better health and quality of life.