Anybody who has had a cold knows how nasty it can get. You might have woken up with a scratchy throat and a stuffy nose, or maybe you are not feeling too well, and your body feels slightly achy. You may even have a fever and cough to deal with. But what if these symptoms don’t go away as you assumed they would? What if it’s not just a common cold and it’s something more serious like pneumonia? How can you tell? Bronchitis or pneumonia share similar symptoms, making it hard to differentiate between them. If your symptoms persist, it is highly advisable to seek the advice and an evaluation by a respiratory specialist.
Exploring the main causes and symptoms of bronchitis and pneumonia: Understanding the similarities and differences
Bronchitis
This respiratory condition occurs when the bronchi, the tubes that carry air into your lungs, get inflamed. Bronchitis usually occurs following a viral infection. Although both bronchitis and pneumonia are often associated with a cough and fever, the fever that comes with bronchitis is usually milder than in pneumonia. Moreover, while pneumonia develops in your lung tissues and gets worse, bronchitis is confined to the bronchial tubes. Other symptoms of bronchitis include cough or chest pain.
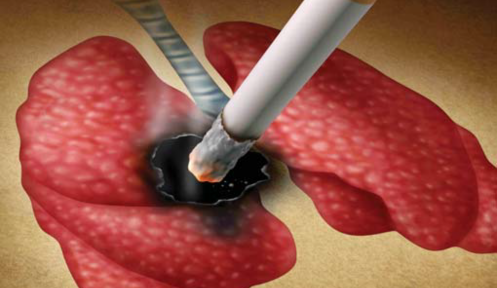
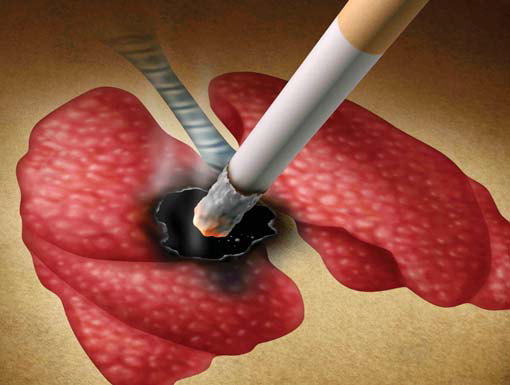
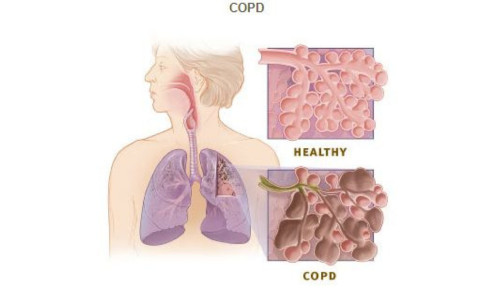
There are two forms of bronchitis: acute and chronic bronchitis. Acute bronchitis occurs suddenly, usually does not last more than a week and seldom recurs. Patients with acute bronchitis often present with a cough with or without sputum. Chronic bronchitis, on the other hand, is a form of COPD (chronic obstructive pulmonary disease) that occurs due to long-term inflammation of the breathing tubes. Smoking is the main cause of this disease and chronic bronchitis is characterised by a chronic productive cough and shortness of breath.
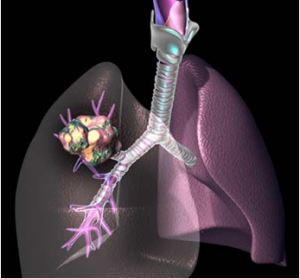
Pneumonia
This respiratory infection develops when the lungs become inflamed, affecting one or both lungs. While anybody can get infected with pneumonia, babies and older adults are at a higher risk of getting seriously ill. In addition, patients with cardiac and other lung conditions like cancer may also be at risk of getting pneumonia. Symptoms may range from mild to serious and may include fever, cough, and breathing difficulties. Bacteria, viruses, and fungi can cause pneumonia and are commonly spread by coughing or sneezing.
Bacteria are the most common cause of pneumonia, and patients often present with a cough that produces thick, yellowish-green sputum with pus. Viral pneumonia is usually mild and comes with symptoms such as fever, dry cough and sore throat. Fungal pneumonia normally occurs in those who have chronic health conditions or a weak immune system such as patients with HIV. This occurs when fungal spores mix with the air we inhale or by the reactivation of a latent infection.
Uncovering the diagnostic and treatment options of bronchitis and pneumonia: Understanding how the conditions are managed

Bronchitis is diagnosed with the help of a detailed medical history and physical examination. In most cases, additional investigations are not required. Some physicians may order a chest X-ray to rule out pneumonia, especially if the patient is very sick. Diagnosing pneumonia can be challenging as the symptoms are often similar to those of a common cold or flu. Therefore, in addition to reviewing your medical history and carrying out a physical examination, your pulmonologist may order a number of tests, including blood tests, chest X-rays and sputum tests. If a patient is in the high-risk group, they may also have to undergo some additional tests like a CT scan, arterial blood gases, bronchoscopy, and a pleural fluid culture.
Most patients with acute bronchitis may not need any treatment as the condition usually resolves on its own. But antibiotics may be needed if it’s bacterial. For chronic bronchitis, the condition results in lung damage and cannot be reversed. If you are a smoker and you quit this habit, the rate of decline will reduce significantly. Bronchodilators are provided to relieve symptoms and relax the airways, while anti-inflammatory drugs may be given to reduce the swelling of the airway passages. Those who have low blood oxygen levels due to lung damage will benefit from oxygen therapy.
Treatment for pneumonia will vary depending on the type of pneumonia and other factors like the patient’s age, health condition, and the severity of the disease. The aim of treatment is to cure the infection and prevent any complications from occurring. Antibiotics will be required for bacterial pneumonia, but if the patient has viral pneumonia, antiviral medication will be prescribed. Antifungal medication will be used in the treatment of fungal pneumonia. If you have mild pneumonia, it can be managed at home, but if the disease is severe, hospitalisation may be required and intravenous fluids, antibiotics, oxygen therapy, and other treatments may be given.
Diving deeper into bronchitis and pneumonia: Can bronchitis turn into pneumonia?
Although both these conditions share many similarities, they are different diseases. Bronchitis usually resolves well with or without treatment while patients with pneumonia need to be treated and followed-up. Those who are at risk of experiencing complications from pneumonia are babies, older adults, and individuals with underlying health conditions and/or a weakened immune system. Therefore, prompt treatment of pneumonia is crucial to prevent complications and a bad outcome.