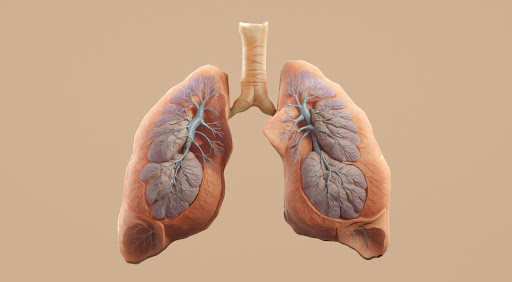
A lung nodule is a small, round, or oval growth in the lung, usually detected during imaging tests such as a chest X-ray or a CT scan. The discovery of a nodule can be quite alarming but not all of them are cancerous. Some are benign and require minimal intervention, while other nodules may require further evaluation by an asthma doctor in Singapore. While asthma itself does not necessarily lead to the formation of lung nodules, certain conditions associated with asthma can do so. Some nodules are a sign of something serious, like infections, inflammation, or even early-stage lung cancer. Understanding the potential causes, symptoms, and risks associated with lung nodules can assist individuals in making informed decisions about their respiratory health.
Common Causes of Lung Nodules
These nodules can develop owing to a multitude of factors, such as:
- Infectious Granulomas: Granulomas are clusters of immune cells that are the most common type of benign nodules. Fungal lung infections or tuberculosis can cause granulomas to form.
- Non-Infectious Granulomas: Autoimmune diseases like rheumatoid arthritis and sarcoidosis can lead to the formation of non-infectious granulomas.
- Benign Tumours: These typically include hamartomas, lipomas, and adenomas.
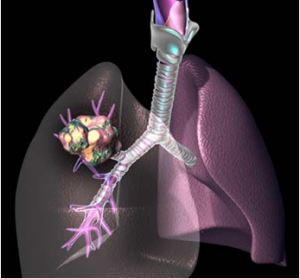
- Cancerous Tumours: A common cause of pulmonary nodules includes non-small cell lung cancer, small cell lung cancer, and carcinoid tumours.
- Fibrotic Scarring: Smoking or inhaling lung irritants or chemicals can lead to lung scarring, which causes nodules.
What Indicates the Presence of a Lung Nodule?
Most nodules do not cause noticeable symptoms, making early detection a bit difficult. However, in cases where symptoms appear, they may include:
- Persistent coughing that lasts a few weeks
- Shortness of breath or difficulty breathing
- Wheezing
- Chest pain that becomes worse with deep breathing or coughing
- Coughing up blood (haemoptysis)
- Hoarseness
- Frequent respiratory infections such as bronchitis or pneumonia
- Unexplained weight loss
- Fatigue
When Should You See a Specialist?
Although most lung nodules are generally harmless, there are certain factors that necessitate immediate evaluation by a doctor, such as:
- History of smoking
- Prolonged exposure to harmful chemicals
- Family history of lung cancer
- The nodule having irregular borders
- The nodule growing over time
- Chronic cough
- Chest pain
Early detection and assessment by an asthma specialist in Singapore can help determine the next course of action including a suitable treatment plan and effective lifestyle changes.
Diagnosis and Testing
When a lung nodule is detected, the specialist may order a series of tests, which include:
- CT Scan: This imaging test provides detailed images of the nodule to assess its size, composition, and shape.
- PET Scan: This test helps determine whether the nodule is active, which can indicate potential malignancy.
- Sputum Cytology: A sputum cytology test involves examining mucus under a microscope to look for abnormal or cancerous cells.
- Bronchoscopy: A thin, flexible tube with a camera is inserted into the airways to collect tissue samples for an analysis.
- Needle Biopsy: A needle is used to extract tissue from the nodule.
Suitable Treatment Options
The treatment approach for lung nodules may differ, depending on the nodule’s size, nature, and potential malignancy. Treatment options typically include:
- Surveillance: Active surveillance, also known as watchful waiting, refers to keeping a close watch on the nodule to see if it grows or changes with time.
- Surgery: This is not required for benign lung nodules, but if a patient has symptoms such as coughing or difficulty in breathing, a specialist may order a biopsy to ascertain what’s causing the development of the nodule. If the test shows that the nodule is cancerous, it can be surgically removed.
Other treatment options for cancerous lung nodules include chemotherapy or radiation therapy.
Consult an Asthma Doctor in Singapore
Although the discovery of a lung nodule can be quite unsettling, they are benign most of the time, depending on the patient’s specific risk factors. If the patient is at risk, however, they should consult a specialist for evaluation, management, and treatment if necessary.
If you or a loved one is experiencing symptoms of a lung nodule, it’s necessary to schedule a consultation with an asthma specialist in Singapore at Philip Eng Respiratory and Medical Clinic. We specialise in the evaluation and diagnosis of a range of lung conditions, to provide evidence-based treatment while prioritising patient comfort and care in a private setting. Led by Dr. Philip Eng, our areas of specialisation include asthma, coughing, wheezing, haemoptysis, and Chronic Obstructive Pulmonary Disease (COPD), emphysema, pneumonia, and suspected lung cancer, among others.
Please feel free to get in touch with us for a consultation. We can be contacted via phone at (+65) 6836 0378 for general enquiries and appointments, or (+65) 6535 8833 for 24-hour answering service. Alternatively, you may email us at drphilipeng@singnet.com.sg or fill out a message form here.